Angina pectoris, commonly known as angina, is a condition marked by chest pain or discomfort due to insufficient oxygen-rich blood reaching the heart muscle. This discomfort often occurs during physical exertion or stress and can significantly impact a person’s quality of life. The underlying cause of angina is typically coronary artery disease (CAD), where the coronary arteries become narrowed or blocked by a buildup of plaque, leading to reduced blood flow to the heart.
Antianginal drugs are a class of medications specifically designed to alleviate the symptoms of angina. Their primary purpose is to improve blood flow to the heart, reduce the heart’s workload, and ultimately relieve chest pain. By targeting the various mechanisms involved in angina, these drugs help manage the condition and improve the overall heart health of patients.
Understanding Angina Pectoris
Overview of Angina and Its Symptoms
Angina manifests as a feeling of pressure, squeezing, or pain in the chest, often radiating to the arms, neck, or jaw. This discomfort is typically triggered by physical exertion, emotional stress, or other factors that increase the heart’s demand for oxygen. Symptoms can vary in intensity and duration but generally subside with rest or medication.
Explanation of Coronary Artery Disease (CAD) and Its Role in Angina
Coronary artery disease is a progressive condition where the coronary arteries, responsible for supplying blood to the heart muscle, become narrowed due to the buildup of fatty deposits called plaque. This plaque restricts blood flow and reduces the amount of oxygen reaching the heart muscle, leading to the characteristic pain and discomfort of angina. CAD is the most common cause of angina and can be exacerbated by factors such as high blood pressure, high cholesterol, smoking, and a sedentary lifestyle.
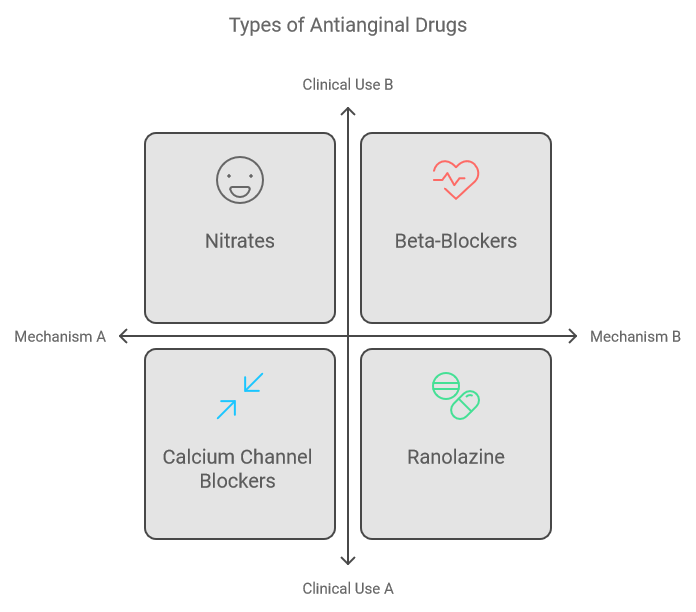
Types of Antianginal Drugs
Nitrates
- Definition and Examples: Nitrates are a group of medications that include nitroglycerin, isosorbide dinitrate, and isosorbide mononitrate. These drugs are used to prevent and relieve angina symptoms.
- Mechanism of Action: Nitrates work by dilating blood vessels, particularly veins, which decreases the amount of blood returning to the heart. This reduces the heart’s workload and oxygen demand. Additionally, nitrates have a coronary vasodilatory effect, enhancing blood flow to the heart muscle.
- Usage: Nitrates are employed both for acute relief of angina attacks and for long-term management. Nitroglycerin can be administered sublingually (under the tongue), topically (via patches), or as a spray for immediate relief. Extended-release forms are available for ongoing control.
Beta-Blockers
- Definition and Examples: Beta-blockers include medications such as atenolol, metoprolol, and propranolol. They are used to manage chronic angina and reduce the frequency of episodes.
- Mechanism of Action: These drugs work by blocking beta-adrenergic receptors, which lowers the heart rate and the force of contraction. This results in decreased oxygen demand and can help prevent angina attacks.
- Usage: Beta-blockers are primarily used for long-term management rather than acute relief. They are effective in reducing the severity and frequency of angina episodes over time.
Calcium Channel Blockers
- Definition and Examples: Calcium channel blockers include amlodipine, diltiazem, and verapamil. They help manage both chronic angina and acute symptoms.
- Mechanism of Action: These medications prevent calcium from entering heart and blood vessel cells, leading to relaxation and dilation of blood vessels. This reduces the heart’s workload and can improve coronary blood flow.
- Usage: Calcium channel blockers are used for both long-term control of angina and immediate relief. They are particularly useful in cases where nitrates or beta-blockers are not suitable or effective.
Ranolazine
- Definition and Mechanism of Action: Ranolazine is a newer antianginal drug that enhances the efficiency of the heart muscle by reducing the amount of sodium and calcium entering heart cells. This helps the heart work more effectively and reduces angina symptoms.
- Usage: Ranolazine is typically used as an adjunct therapy in chronic angina when other medications are not sufficient to control symptoms.
This detailed examination of antianginal drugs provides a comprehensive understanding of their role in managing angina and improving heart health.

Combining Antianginal Drugs
Combination Therapy: How Different Drugs May Be Used Together for Comprehensive Management
In managing angina pectoris, often a single type of antianginal drug is not sufficient to provide complete relief. Combining different types of antianginal drugs can enhance the overall effectiveness of treatment. Each class of drug works through distinct mechanisms to alleviate angina symptoms, making combination therapy a powerful strategy for comprehensive management. For instance, while nitrates improve blood flow and reduce heart workload, beta-blockers decrease heart rate and oxygen demand. Using these drugs together can address multiple aspects of angina simultaneously.
Examples of Combinations: Nitrate with Beta-Blocker or Calcium Channel Blocker
- Nitrate and Beta-Blocker: Combining nitrates with beta-blockers is a common approach. Nitrates provide rapid relief from acute angina attacks, while beta-blockers are effective for long-term prevention. This combination helps manage both immediate symptoms and reduces the frequency of angina episodes over time.
- Nitrate and Calcium Channel Blocker: When a nitrate is combined with a calcium channel blocker, the result is a synergistic effect that enhances blood vessel dilation and reduces heart workload. This combination is particularly useful for patients whose angina is not well-controlled by nitrates alone.
Benefits of Combination Therapy: Improved Symptom Control and Management of Angina
Combining antianginal drugs offers several benefits:
- Enhanced Effectiveness: By targeting different pathways involved in angina, combination therapy often leads to better symptom control than any single drug alone. This can result in a more significant reduction in the frequency and severity of angina episodes.
- Reduced Drug Dosage: Using multiple drugs in combination can allow for lower doses of each medication. This approach can minimize potential side effects and improve patient tolerance.
- Comprehensive Management: Combination therapy addresses both the immediate and long-term aspects of angina management. Nitrates provide quick relief, while beta-blockers and calcium channel blockers contribute to sustained control and prevention.
- Tailored Treatment: Combining drugs allows for a more personalized treatment approach, as healthcare providers can adjust the combination based on individual patient needs and responses.
Conclusion
Antianginal drugs play a crucial role in managing angina pectoris by alleviating symptoms and improving heart health. Understanding the different types of antianginal drugs—nitrates, beta-blockers, calcium channel blockers, and ranolazine—along with their mechanisms and uses, is essential for effective treatment. Combining these drugs can further enhance symptom control and offer a more comprehensive approach to managing angina.
For optimal results and personalized treatment plans, it is important to consult healthcare providers. They can tailor therapy based on individual health conditions, response to medications, and specific needs, ensuring the most effective management of angina.
Frequently Asked Questions (FAQs)
1. What are antianginal drugs used for?
Antianginal drugs are used to treat angina pectoris, a condition characterized by chest pain or discomfort due to reduced blood flow to the heart muscle. These medications help alleviate symptoms of angina, improve blood flow to the heart, and reduce the heart’s workload.
2. How do nitrates relieve angina symptoms?
Nitrates relieve angina symptoms by dilating blood vessels, particularly veins. This reduces the amount of blood returning to the heart, lowering the heart’s workload and oxygen demand. Nitrates also help to improve blood flow to the heart muscle, providing quick relief from angina attacks.
3. What are the common side effects of beta-blockers?
Common side effects of beta-blockers may include fatigue, dizziness, cold hands or feet, and a slow heart rate. Some individuals might also experience weight gain or mood changes. It’s important to discuss any side effects with your healthcare provider.
4. When should calcium channel blockers be used?
Calcium channel blockers are used both for long-term control of angina and for immediate relief. They are particularly helpful for patients who do not respond well to nitrates or beta-blockers. They work by relaxing and dilating blood vessels, which reduces the heart’s workload.
5. How does ranolazine differ from other antianginal drugs?
Ranolazine works differently from other antianginal drugs by improving the efficiency of the heart muscle. It reduces the amount of sodium and calcium entering heart cells, which helps the heart work more efficiently. Ranolazine is often used as an adjunct therapy when other medications alone are not sufficient.
6. Can antianginal drugs be combined with other medications?
Yes, antianginal drugs are often used in combination with other medications to provide comprehensive management of angina. Common combinations include nitrates with beta-blockers or calcium channel blockers. This approach helps to target different mechanisms involved in angina and improve overall symptom control.
7. What are the benefits of combination therapy for angina?
Combination therapy can enhance the effectiveness of treatment, reduce the need for higher doses of each medication, and provide more comprehensive symptom management. It also allows for a more personalized approach to treatment based on individual patient needs.
8. Are there any lifestyle changes that can complement antianginal drug therapy?
Yes, lifestyle changes such as maintaining a healthy diet, engaging in regular physical activity, quitting smoking, and managing stress can complement antianginal drug therapy. These changes can help improve overall heart health and reduce the frequency and severity of angina episodes.
9. How should I use nitrate medication for acute angina attacks?
Nitrate medications for acute angina attacks, such as nitroglycerin, can be administered sublingually (under the tongue), as a spray, or through patches. Follow your healthcare provider’s instructions for the correct dosage and method of administration. Typically, these medications provide quick relief from angina symptoms.
10. How often should I follow up with my healthcare provider while on antianginal medication?
Regular follow-ups with your healthcare provider are important to monitor the effectiveness of the medication, adjust dosages if needed, and manage any side effects. Your provider will recommend a schedule based on your specific condition and response to treatment.
